How can we regenerate tissues that are damaged, lost or diseased in the human body? This was the central question driving the four scientists who presented their research at the Junior Faculty Candidate Seminar and Symposium, hosted by USC’s Department of Stem Cell Biology and Regenerative Medicine.
At a February 10 seminar, Kyle McCracken, MD, PhD, from Boston Children’s Hospital and Brigham and Women’s Hospital, shared progress in regenerating one of the least regenerative organs in the body: the kidney. McCracken described how he directed human stem cells to form kidney-like structures known as organoids.
“In my first year as a medical student, learning about renal physiology was really my inspiration for wanting to do nephrology. It’s so complicated and so amazing, and it makes so much sense that I never could stop thinking about it,” he said.
By relying on the body’s natural developmental signals, McCracken successfully grew organoids that resembled the collecting duct that helps maintain the body’s fluid and pH balance, and concentrates and transports urine. Strikingly, the organoids showed the kidney’s branching architecture. Some of the cells even acquired basic functions, such as transporting salt and creating pH gradients.
“The ability to differentiate good kidney tissues from stem cells is going to open up a huge amount of opportunity, scientifically and translationally, in the field of nephrology,” said McCracken.
Organoids serve as models of development and disease, platforms for screening drugs to treat kidney disease, and a first step towards generating functional replacement tissues for patients.
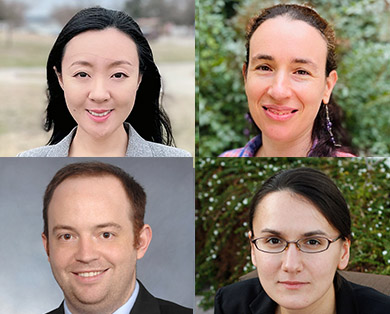
At the March 8 symposium, three scientists provided new insights into their research on heart regeneration, hair follicle stimulation, and developmental pathways that drive limb regeneration in amphibians.
Miao Cui, PhD, from the University of Texas Southwestern Medical Center discussed how newborn mice regenerate their hearts after severe injuries, such as heart attacks. This remarkable regenerative ability is lost one week after birth, which is part of the reason why heart disease is the leading cause of death in the United States.
“We think that, with regenerative medicine , , we can find mechanisms that can fully repair and regenerate the lost or damaged tissue,” said Cui, “and it would be the most effective way to treat heart disease.”
With this goal in mind, Cui has undertaken a detailed study of the molecular and cellular factors that contribute to the newborn mouse’s ability to regenerate its heart. Near the site of heart injury, she has identified a highly regenerative population of heart muscle cells, with embryo-like gene activity that enables survival and proliferation in stressful, low-oxygen conditions. She has also observed that newborn mouse hearts have a very limited post-injury inflammatory response.
“In my future research, I’d like to use several genomics and systems biology tools to study the developmental signals and injury-induced responses that allow the neonatal heart to regenerate,” she said.
Yulia Shwartz, PhD, from Harvard University examined how environmental changes—such as cold temperatures—can affect stem cells in the skin.
“When it comes to the skin, one of the most evolutionarily conserved reactions is the goosebump reaction, which is piloerection,” she said.
When it gets cold, the nerves send a message to a tiny muscle, called the arrector pili, located at the base of the hair follicle. As this muscle contracts, it creates the goosebump that raises the hair, providing extra warmth.
Shwartz discovered that when mice are exposed to two weeks of cold, the nerves stimulate not only the contraction of the arrector pili muscle, but also the activation of the stem cells in the follicle to grow more hair—thus keeping the animal warm.
“Working on the skin, there are multiple different environmental changes, and they can lead to multiple systemic effects. How all these systemic effects eventually converge to regulate stem cell behavior is one of the questions I’m most fascinated about,” she said. “And it will give us an idea or better understanding of not only stem cell biology, but also how we can harness stem cells in order to combat wound healing or aging.”
Olena Zhulyn, PhD, from Stanford University talked about translation, or how an organism uses genetic instructions to make the proteins it needs to build itself during embryonic development or repair itself after an injury such as a limb amputation. Specifically, Zhulyn focused on how an organism regulates this important process of translation, thus synthesizing either greater or lesser quantities of a given protein.
“When you think about protein synthesis, it’s the last step in the journey from a gene to a protein product,” said Zhulyn, “And my thinking was that if we look at the last step of this journey, we might get a more direct understanding of what is necessary for a process.”
When an embryo is forming, translational regulation allows an organism to rely on a small number of key developmental genes, such as SHH and WNT, to construct a vast diversity of anatomical structures.
Zhulyn also examined translational regulation in the context of one of the most striking examples of vertebrate regeneration: the axolotl salamander’s ability to regrow a severed arm. Following injury, the axolotl relies on a protein called mTOR to activate translation, increasing protein synthesis. In contrast, a mouse, which is unable to regrow an amputated finger, has a different form of mTOR that does not increase translation following injury.
The axolotl “is actually a very beautiful model to study scarless wound healing,” said Zhulyn. “I very much would love to pursue that in order to use the axolotl as a springboard to really promote better wound healing in mammalian tissues.”
Andy McMahon, PhD, FRS, chair of USC’s Department of Stem Cell Biology and Regenerative Medicine, thanked the scientists for their terrific talks.
“It’s been delightful to meet you,” he said, “and to hear about your wonderful science.”
