Researchers from the Keck School of Medicine of USC, in collaboration with Baylor College of Medicine in Houston, Texas, used an innovative imaging tool to examine the mouse inner ear and made a discovery that could help treat hearing disorders.
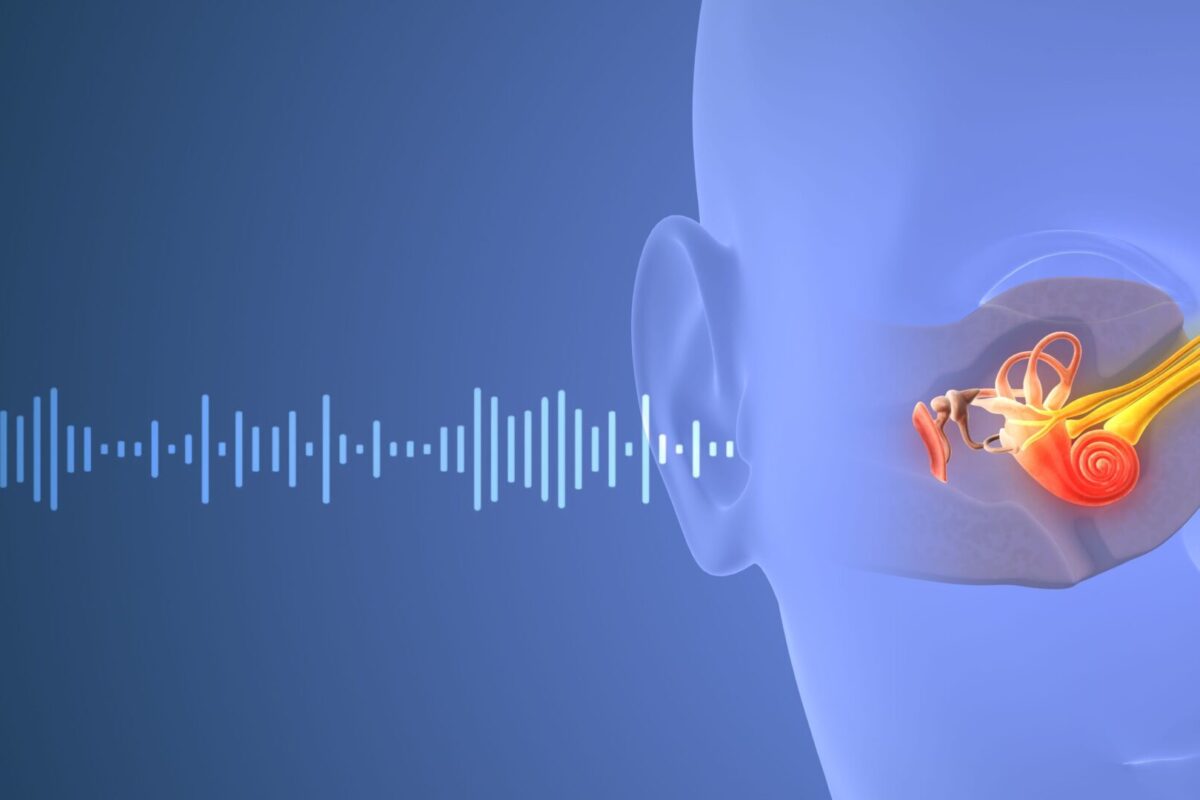
The brain may play a role in helping the ear regulate its sensitivity to sound and compensate for hearing loss by sending a signal to a structure in the inner ear known as the cochlea, according to a study that was just published in the Journal of Neuroscience. The discovery could help researchers develop treatments for tough-to-treat hearing disorders such as hyperacusis, where everyday sounds seem uncomfortably loud, and tinnitus, a sensation of ringing, buzzing or other sound in the ear when there is no external source.
The findings were powered by a new imaging tool, which allowed scientists to collect images of the cochlea in awake animals for the first time.
The cochlea uses sensory hair cells to detect sound waves in the air, then converts them into electrical signals that the brain can process. Most cochlear nerves carry information from the cochlea to the brain, but about 5% send signals in the opposite direction: from the brain to the cochlea. The exact role of those fibers has been a mystery, because researchers have struggled to measure cochlear activity in humans or animals while they are awake.
To change that, researchers from the Keck School of Medicine of USC, in collaboration with Baylor College of Medicine in Houston, Texas, have developed a new way to look at activity in the inner ear by adapting an imaging technique called optical coherence tomography (OCT), which is widely used in ophthalmology offices to scan the retina for conditions like glaucoma and macular degeneration. OCT uses light waves to scan tissue and create a 3D image, similar to the way ultrasound creates images from sound waves. Using this approach, the researchers captured real-time images of the cochlea in action.
“OCT lets us look down the ear canal, through the eardrum and bone into the cochlea, and measure how it’s working—noninvasively and without pain,” said John Oghalai, MD, professor and chair of otolaryngology-head and neck surgery and the Leon J. Tiber and David S. Alpert Chair in Medicine at the Keck School of Medicine. “What’s exciting about this is it lets us study how the brain is controlling the cochlea in real time.”
Using this tool, Oghalai and his team, including co-leaders Patricia Quiñones, PhD, research associate in Oghalai’s Lab, Brian E. Applegate, PhD, professor of otolaryngology-head and neck surgery at the Keck School of Medicine, and Matthew J. McGinley, PhD assistant professor at Baylor College of Medicine, found that in healthy mice, cochlear activity does not change over the short term. But in mice with genetic hearing loss, cochlear function increased, indicating that the brain was enhancing the cochlea’s sensitivity as a response to long-term hearing loss.
Measuring cochlear function
A leading theory about the nerves that send signals from the brain to the cochlea (known as “efferent” fibers) is that they control the cochlea’s response to sound on a short-term basis, similar to the way our pupils work. Bright light makes the pupils constrict, while stress causes them to dilate. Could the cochlea be acting in a similar way?
To explore whether the cochlea responds to short-term stimuli, the researchers measured cochlear activity in mice using OCT. At the same time, they tracked the shifting brain states of the mice by measuring changes in pupil size. As brain states changed, cochlear activity stayed the same, suggesting that the inner ear does not modulate hearing on a short-term basis.
Next, the researchers genetically altered mice to disable the nerves carrying information from the inner ear to the brain (“afferent” fibers), causing hearing loss. Using OCT, they found that the cochlea was working overtime to compensate.
“As humans age and our hair cells die off, we start to lose our hearing. These findings suggest that the brain can send signals to the remaining hair cells, essentially telling them to turn up the volume,” said Oghalai, who is also a professor of biomedical engineering at the USC Viterbi School of Engineering.
The next step is a clinical trial to test drugs that block efferent fibers, which could lower the volume for patients with hyperacusis and may also help address tinnitus.
Improving diagnosis
OCT also holds promise for improving the diagnosis and treatment of hearing disorders. Now that Oghalai’s team has adapted OCT for cochlear imaging in awake mice, they are testing a version of the tool for patients in a new NIH-funded study.
The technology could ultimately allow providers to diagnose hearing problems based on physiology, not just performance on a hearing exam, and to tailor treatments to individual needs.
“This is the first step toward a tool that lets us look into a patient’s ear, find out what the problem is and treat it,” Oghalai said.
About this research
In addition to Oghalai, the study’s other authors are Patricia M. Quiñones, Michelle Pei, Ariadna Cobo-Cuan, Marcela A. Morán, Bong Jik Kim, Clayton B. Walker, Michael J. Serafino, Frank Macias-Escriva, Juemei Wang, James B. Dewey and Brian E. Applegate from the Caruso Department of Otolaryngology-Head and Neck Surgery, Keck School of Medicine of USC, University of Southern California; and Hemant Srivastava and Matthew J. McGinley from the Department of Neuroscience, Baylor College of Medicine, Houston, Texas and the Duncan Neurological Research Institute, Texas Children’s Hospital, Houston, Texas.
This work was supported by the National Institute on Deafness and Other Communication Disorders [R01 DC014450, R01 DC013774, R01 DC017741, R25 DC019700, R21 DC019209, R01 DC017797]; the National Institute of Biomedical Imaging and Bioengineering [R01 EB027113]; and the Keck School of Medicine Dean’s Research Scholar Program.
Disclosure: John Oghalai and Brian Applegate are founders of AO technologies, with the goal of translating inner ear imaging technologies for clinical purposes.
