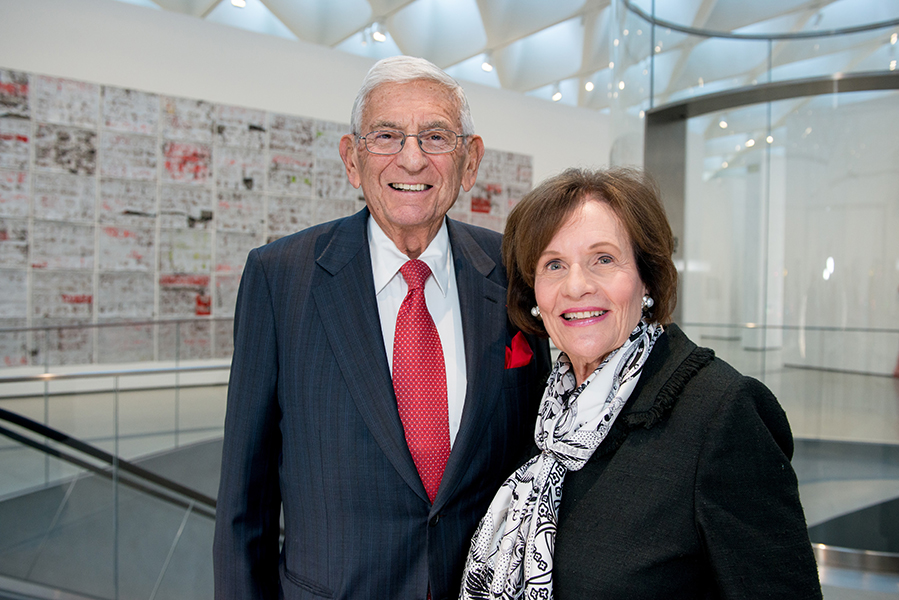
Last Friday, scientists from USC, UCLA and UCSF gathered at a symposium to celebrate the tenth anniversary of their three stem cell research centers, established with support from Eli and Edythe Broad and the California Institute for Regenerative Medicine (CIRM). As the guests of honor, the Broads marked the milestone by surprising the centers with a $1 million gift to support eight grants for early-stage stem cell research projects.
“We love scientists because none of you are satisfied with the status quo,” said Eli Broad at the symposium, hosted by UCLA.
As the director of UCLA’s stem cell research center, Owen Witte expressed his gratitude: “It’s hard to put into a simple sentence how important this philanthropy has been for all three of our centers. But I can honestly say that without their philanthropy to help establish these three sites, I don’t think UCLA would have accomplished what we’ve been able to, and I’m pretty sure the same holds true for USC and UCSF.”
Arnold Kriegstein, director of UCSF’s stem cell research center, acknowledged the Broads’ contribution to their “thriving stem cell enterprise.”
Andy McMahon, director of USC’s stem cell research center, highlighted the Broads’ enormous influence not only on science, but also on art and education.
“Art, education and science hold special and personal meanings for us all,” said McMahon. “Through art, we explore our imaginations. Through education, we realize our potential. Through science, we improve our lives. And through the Broads’ lifelong and transformative philanthropy, art and education and science have flourished to the great and obvious benefit of all.”
In addition to recognizing the Broads, the symposium highlighted recent scientific progress in regenerative medicine.
UCLA’s Donald Kohn described how stem cell research has already cured infants born without a functional immune system—an inherited condition called Adenosine Deaminase Severe Combined ImmuneDeficiency (ADA SCID), or “Bubble Baby Disease.” The traditional treatment is a bone marrow transplant, also known as a hematopoietic stem cell (HSC) transplant, from a matched donor—which carries significant risk of fatal immune rejection or other complications. Kohn’s lab engineered a better source of transplanted cells: the patients’ own HSCs, in which the disease-causing mutation has been corrected using gene editing. This cure already proved successful in clinical trials, and is now being commercialized with support and funding from CIRM.
Kriegstein shared how his stem cell research spurred an ongoing clinical trial, using the antibiotic Azithromycin as a treatment for Zika patients in Brazil. He discovered the anti-Zika action of this common antibiotic by testing it on stem cell-derived brain cells. In particular, his research has focused on a highly proliferative cell type: the Outer Subventricular Zone Radial Glial Cell (oRGs), which contribute to the massive expansion of the human brain during development. This cell type is implicated not only in Zika-induced microcephaly, but also in the fatal adult brain tumor glioblastoma and the developmental disorder lissencephaly.
UCSF’s Holger Willenbring is also nearing the clinical trial stage with a stem cell-based approach to treating liver scarring, also known as fibrosis or cirrhosis. In hopes of reversing the condition, his lab has pioneered gene therapy to transform fibrotic myofibroblasts, which take over the diseased liver, into healthy liver cells. To facilitate this approach, the team developed a highly effective way to deliver this gene therapy directly to the liver in their model of human disease: using a specific type of delivery vehicle or vector, known as an adeno-associated virus (AAV) serotype 6.
Other scientists shared projects at any earlier stage of research and discovery. They painted a vision of a future in which kidney disease, hearing loss, cancer, infertility and even aging itself could become afflictions of the past.
McMahon underscored the need for more scientists to dedicate their energies to helping the transplant patients who can’t obtain kidneys due to the severe donor shortage. To begin addressing this problem, he has focused his lab’s full efforts on using stem cells to generate a human nephron, the functional unit of the kidney. To better understand how a human nephron develops, his lab is studying organoids, 3D assemblies of cells possessing rudimentary kidney structure and function.
UCSF’s Saul Villeda raised a universally relevant question: can we reverse the effects of aging on cognitive function? The answer could be yes. In the blood of old mice, his lab showed that elevated levels of B2M have as a “pro-aging” effect in the brain, decreasing the birth of new neurons and impairing spatial learning and memory. In the blood of young mice, they found a “youthful” factor called “Tet2,” which stimulates the birth of neurons and supports cognitive function.
Also in the neurosensory realm, USC’s Neil Segil addressed hearing loss, which affects approximately 10 percent of the world’s population and half of the retirement-aged population. Most hearing loss is due to damage to the inner ear’s sensory cells, which do not regenerate in humans. However, they do regenerate in non-mammals, such as birds—thanks to a population of neighboring cells that respond to deafness by differentiating into replacement sensory cells. Segil’s group is exploring ways to stimulate a similar regenerative response in mammals.
The mutations underlying cancer were the topic for USC researcher Min Yu. Her lab studies patient-derived breast cancer stem cells (CSCs), which break off of the primary tumor, enter the blood stream and seed the new metastatic tumors that ultimately prove fatal. In analyzing these CSCs, her lab found that certain mutations and gene activity can consistently predict specific patterns of metastasis—such as the formation of secondary tumors in the brain versus other organs. These insights could inform the future of personalized medicine.
Witte shared his insights into metastatic prostate cancer, which typically develops resistance to traditional therapies. By studying patients’ bone metastases, his lab found that many prostate cancers start off as less aggressive adenocarcinomas and then transmogrify into more malignant small cell carcinomas. By characterizing these cells, his lab is paving the way for targeted treatments for advanced prostate cancer.
UCLA’s Amander Clark discussed how young cancer patients often become infertile from treatments such as radiation and chemotherapy. To tackle this problem, her lab is reprogramming primate skin cells into the two types of germline cells: eggs and sperm. So far, they’ve succeeded in producing what they call primordial germ cell-like cells (PGCLCs)—which are precursors to fully developed eggs and sperm. They are now testing if these cells continue to develop into mature, functional germline cells when transplanted into living organisms.
“Edye and I want to thank each of you for your dedication,” said Eli Broad. “We cannot express how much your work means to us and how we appreciate all you do to improve human health.”
