USC Stem Cell scientists discover a new way to rid cells of toxic tau protein in a study involving mice and lab-grown human “mini-brains,” known as organoids.
The neurotransmitter glutamate is essential for regulating everything from mood to memory, but it can also encourage a toxic buildup of the notorious tau protein, which can contribute to Alzheimer’s and related diseases. In a USC Stem Cell-led study published in Neuron, scientists describe a new approach for counteracting these devastating and often fatal neurodegenerative effects.
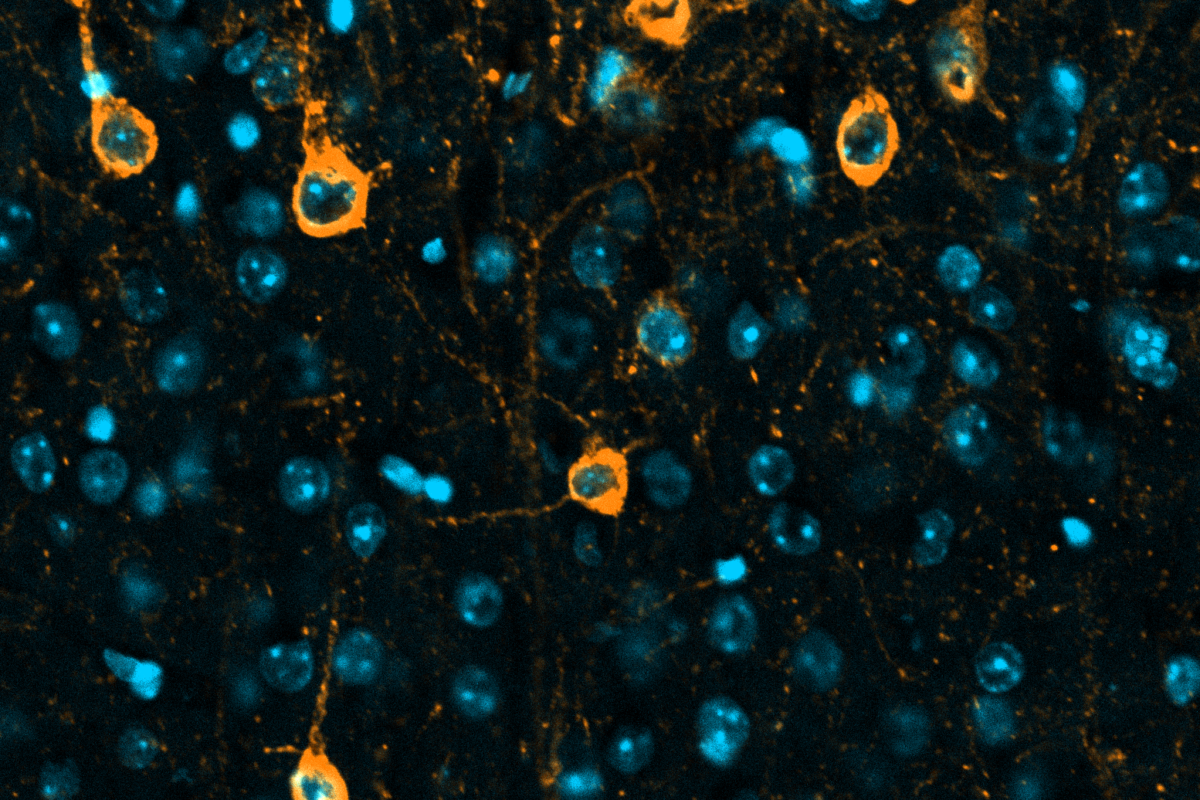
In the study, first authors Joshua Berlind and Jesse Lai made their discovery by studying lab mice as well as human brain “organoids,” which are rudimentary brain-like structures grown in the lab. The scientists produced these organoids from stem cells derived from healthy people as well as from patients with neurodegenerative diseases related to tau toxicity.
When exposed to glutamate, the organoids—particularly the ones derived from patients with neurodegenerative diseases—exhibited a toxic buildup of tau protein as well as neurodegeneration and nerve cell death. Mice with a mutation in tau, which causes a common form of dementia, displayed similar pathologies.
“Many potential drugs have been developed to mitigate the neurodegenerative effects of glutamate toxicity, but they’ve had mixed results in clinical trials,” said corresponding author Justin Ichida, who is the John Douglas French Alzheimer’s Foundation Associate Professor of Stem Cell Biology and Regenerative Medicine at the Keck School of Medicine of USC, a New York Stem Cell Foundation-Robertson Investigator, and a USC Merkin Scholar. “One challenge is that directly limiting the activity of glutamate, a key neurotransmitter, can have negative consequences, such as motor or memory deficits or even reduced consciousness.”
Taking a different approach, the scientists screened for genes that respond to glutamate and identified a gene called KCTD20. When the scientists suppressed the activity of this gene in the organoids and in the mice, glutamate did not produce the same ill effects in terms of either tau buildup or neurodegeneration.
Through additional experiments, the team discovered that suppressing this gene activated cellular compartments called lysosomes, which enveloped the toxic tau proteins and expelled them from the organoids’ cells.
“Our study points towards enhancing tau protein clearance as an important therapeutic strategy, rather than aiming to limit glutamate activity,” said Lai, who completed his postdoctoral training in the Ichida Lab and Amgen and now works at Dewpoint Therapeutics.
Berlind, a postdoc in the Ichida Lab, added: “This is a promising new direction for developing targeted treatments for patients with tau-related neurodegenerative diseases including Alzheimer’s disease.”
Additional co-authors include: Cecilia Lie, Jokabeth Vicente, Kelsey Lam, Sheron Guo, and Jonathan Chang from USC; and Violeta Yu from Dewpoint Therapeutics.
This work was supported by federal funding from the National Institutes of Health (grants NINDS/NIA F31NS117075 and NINDS 1R01NS097850-01) and the Department of Defense (grant 12907280). Additional support came from an Amgen postdoctoral fellowship, the New York Stem Cell Foundation, the Tau Consortium, the Harrington Discovery Institute, the Alzheimer’s Drug Discovery Foundation, the Association for Frontotemporal Dementia, and the John Douglas French Alzheimer’s Foundation.
Disclosures
Lai and Yu are currently employees of Dewpoint Therapeutics and were employees of Amgen during the study. Ichida is a co-founder of AcuraStem and Modulo Bio, a Scientific Advisory Board (SAB) member at Spinogenix, Synapticure, and Vesalius Therapeutics, and a member of the Research and Early Development group at BioMarin Pharmaceutical. All other authors have no conflicts of interest to declare. Named companies were not involved in this project.
