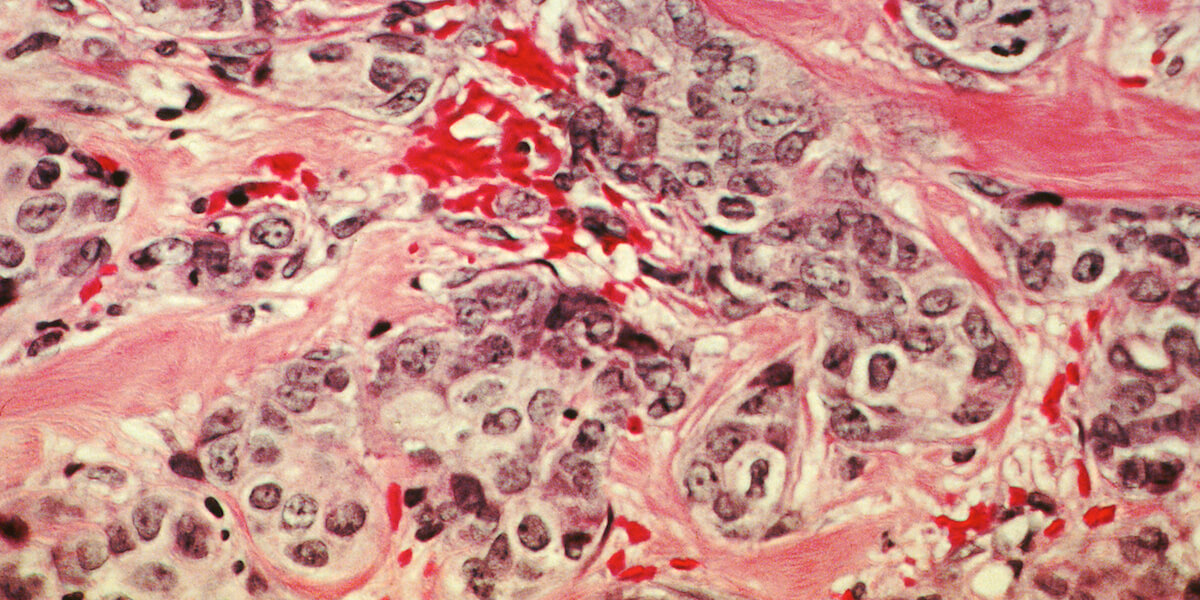
Cancer is the world’s second leading cause of mortality. According to the World Health Organization, it was responsible for around 9.6 million deaths in 2018. Yet over 90 percent of cancer deaths are not caused by the original tumor or disease. They are instead caused by the processes of metastasis; the spread of cancer or tumors leading to secondary growths, often in other parts of the body away from the primary source.
The $2 million grant headed by Assistant Professor of Biomedical Engineering Keyue Shen, funded by the Provocative Questions Initiative at the National Cancer Institute, will aim to increase our understanding of the way cancer behaves and how it spreads. The ultimate goal: to stop metastasis in its tracks and reduce the mortality rate of cancer.
“We’re looking at a new perspective to treat the disease,” Shen said. “The aim would be to prevent metastasis by regulating the cancer cells through the tumor microenvironment, with something that can suppress the cells’ transition from dormant cells to malignant cells.”
Shen said that medical research has barely scratched the surface of how metastasis occurs. He said that recent research in the field has focused on how the metastasis is related to the mitochondria, the power house of our cells, which can turn sugars, fats and proteins into energy.
“In recent years we have realized more and more that mitochondria plays a very important role in cancer cell behaviors,” Shen said.
He said that for a long time, a prevailing thought was that there was a problem with mitochondria in cancer cells, leading to the excessive consumption of glucose outside the mitochondria for energy production.
“Now we are realizing that mitochondria in cancer cells are still functional and still participating in energy production as well as cell signaling and dictating cell behavior,” Shen said. “One thing that people have noticed is that there is actually more production of new mitochondria in metastatic tumor cells circulating in the blood.”
Shen said that mitochondria have multiple membranes that allow them to produce energy through “mitochondrial membrane potential” – a difference in electrical potential between the interior and exterior of the mitochondria, but that cancer cells have an elevated potential compared to normal cells.
“People don’t know exactly what’s causing this. People know that this is related to more aggressive behaviors in cancer cells but they have not really associated that with the ability of the cancer cell to metastasize,” Shen said.
Assistant Professor Keyue Shen. Photo credit/Viterbi Staff
Shen and his research group recently created a model of tumors in a dish where the cancer cells were surrounded by genetically normal connective tissue cells (stromal cells) that commonly appear in tumors, so they could see how the cancer interacted with the surrounding tissue. They also created an environment deficient of oxygen, a key ingredient of mitochondrial respiration, to some regions of cells in the model.
“It was very much mimicking what’s happening in the real tumors,” Shen said.
“The cancer cells that were close to the stromal cells have higher respiration rate and mitochondrial membrane potential and also production of new mitochondria, while the ones that were further away have lower levels of these activities,” he said.
“One of the research topics I have been looking at is studying this tissue interface between cancer cells and stromal cells and the oxygen environment to see what influence they have in terms of cancer progression.”
Shen and his team will also collaborate with Min Yu, Assistant Professor of Stem Cell & Regenerative Medicine from Keck School of Medicine of USC, and Changhan Lee, Assistant Professor at USC Leonard Davis School of Gerontology, to study the behavior and mitochondrial features of migratory cancer cells and those circulating tumor cells in the blood. These are cells that are shed from the primary tumors and are distributed elsewhere in the system where they metastasize. To achieve this, the team will use cancer cells from patients, to study the mitochondria of these cells both in the dish and implanted in mice.
“It’s a five year grant that will really allow us to explore this question, and in the long run enable us to develop our research program here,” Shen said.
The latest grant builds upon Shen’s previous work funded through a Marni Levine Memorial Research Career Development Award from STOP CANCER, a research grant from the Phi Beta Psi Sorority, an Eli and Edythe Broad Innovation Award from the Broad Foundation, a Rose Hills Research Fellowship from the Rose Hills Foundation, and an NIH Trailblazer Award from the National Institute of Biomedical Imaging and Bioengineering.
