With a $2.3 million NIH award, USC researchers will study how cilia behavior and structure impact their function, a key in improving diagnostics and treatments for lung illnesses like COVID-19.
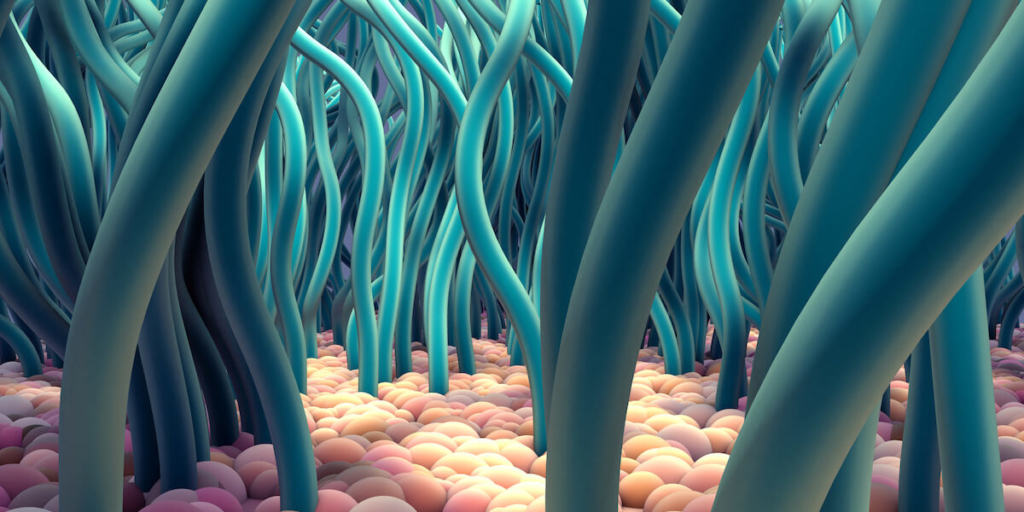
Cilia, microscopic hairlike structures found along the bronchi (air passages throughout the lungs), are the first line of defense against environmental pollutants, viruses and bacteria. But we know little about how they are arranged, how they move or even how they are oriented—all factors which likely impact how well they defend and protect our airways.
With support from the National Institutes of Health, researchers from the USC Viterbi School of Engineering and the Keck School of Medicine of USC are working to bridge mathematical models of cilia behavior to biological and pathological (disease-causing) consequences. In other words, they hope to better understand how changing a variable in how cilia beats or how it is spaced might impact an individual’s health.
The research leads are Eva Kanso, USC Viterbi professor of aerospace and mechanical engineering, and Amy Ryan, PhD, an assistant professor of medicine at the Keck School.
Kanso, Zohrab A. Kaprielian Fellow in Engineering, said: “We want to first understand what the normal variations for healthy lungs are, then understand the pathological variations. If we can map these observations to the underlying pathology, we can understand better how structure of cilia—distribution, coordination, polarity, density—can impact actual function—how they move mucus, how well they clear in a certain direction.”
The team is looking at cilia from three perspectives, Kanso said. “First, we’re looking at actual human lungs, which is very timely now considering COVID-19,” she said. “There are so many questions we don’t know the answer to, like the distribution of cilia from the upper airways to when they start to branch out into smaller branches. Distribution varies depending on where you are in the lung.
Mathematical Modeling of Cilia to Answer Key Questions
In Kanso’s lab, this exploration is being done through mathematical models. “We have models of individual cilia and we combine them together to look at the coordination of an array of cilia. We look at the function and transporting flow, manipulating all sorts of parameters,” she said.
Cilia coordinate spontaneously to create a wave pattern, Kanso said, which is important for the transportation of fluid. “There is a clear direction in which the wave is traveling and that sweeps out everything (bacteria, etc.) in the direction of that traveling wave.”
In the mathematical model, Kanso said, you can change spacing between cilia, individual beating, polarity, etc. and see how it shifts the coordination that emerges and ultimately the corresponding function of the cilia and its transporting flow. Parameters that negatively impact the wave pattern might yield clues as to how diseased lungs look and function, she said.
Implications for Human Health
From the biological perspective, this research could provide significant new insights into inherited and acquired airway diseases characterized by dysfunction of the cilia, Ryan said.
“In addition to substantially increasing our understanding of the impact of disease on the functional properties of the airways, the development of mathematical models could potentially be applied in ciliopathy diagnostics to predict disease progression.” Current diagnostic techniques require very specific scientific expertise, Ryan said, making them challenging.
“Looking forward, our long-term goal is to combine lab models with computational models to create a medical tool that can help evaluate therapeutics targeting lung diseases characterized by poor mucociliary clearance—or poor functioning of self-clearing methodology in the airways,” Ryan said.
The NIH award is over $2.3 million for four years.
