Cutbacks in National Institutes of Health (NIH) funding have made the climate for new research challenging. Three studies from investigators in the Department of Medicine at the Keck School of Medicine of USC have bucked this trend, receiving NIH grants. The researchers — Heinz-Josef Lenz, MD; Michael Kahn, PhD; Laurie D. DeLeve, MD, PhD; and Zea Borok, MD — are all principal investigators with USC Stem Cell, a university-wide, multidisciplinary initiative working to translate the potential of stem cell research to the clinical imperative of regenerative medicine.
Lenz, professor of medicine and preventive medicine and co-director of the Colorectal Center, and Kahn, Provost Professor of Medicine and Pharmacy, recently received an NIH grant of $2.2 million over five years for their study, “Efficacy of Novel Wnt Modulator in Colon Cancer.”
According to Lenz and Kahn, 80 to 90 percent of colorectal cancers involve aberrant activation of the Wnt/beta-catenin signaling pathway, which is connected to tumor initiation, proliferation, progression and poor prognosis. Wnt/beta-catenin is also important in the maintenance, proliferation and differentiation of embryonic and adult somatic stem cells.
Genetic coactivators CBP and p300 have distinct functions in regulating Wnt/beta-catenin-regulated gene expression. Lenz and Kahn believe that increased CBP/beta-catenin/TCF4 transcription at the expense of p300/beta-catenin/TCF4-mediated transcription is associated with colon cancer development, and is a main cause for tumor relapse, drug resistance, metastases and poor prognosis.
“This research has the potential to change the way we treat colon cancer in the future,” said Lenz. “It addresses for the first time the most important and most frequent underlying colon cancer signaling pathways for the first time, which [are] the ultimate reason our treatments fail. We finished the first human clinical trial and presented the results in June 2013; the first randomized trial in colon cancer patients will happen this year.”
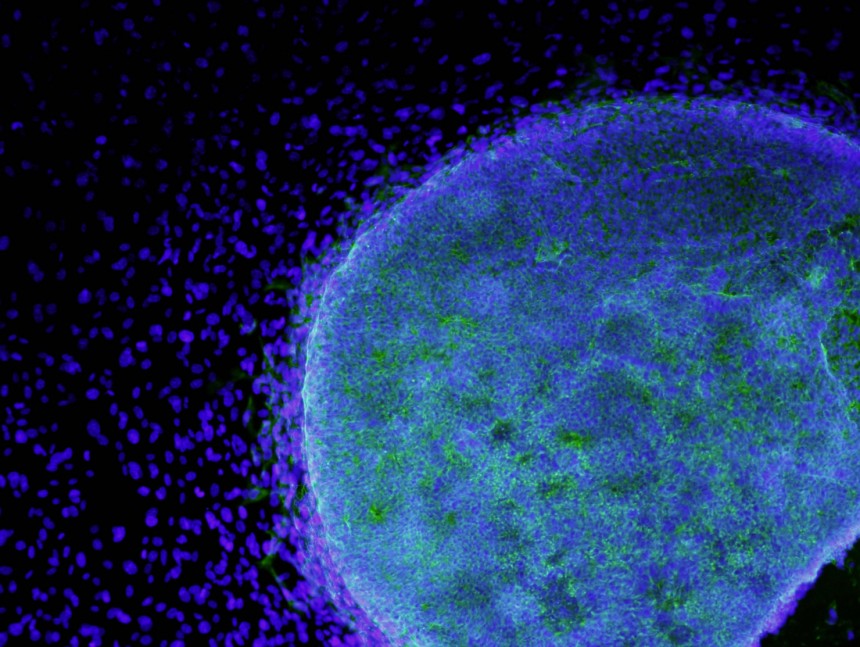
DeLeve, professor of medicine in the division of gastrointestinal and liver disease, received an NIH grant for $356,700 for her study, “Liver Sinusoidal Endothelial Cell Progenitor Cells.”
There are two types of liver sinusoidal endothelial cell (LSEC) progenitor cells: bone marrow LSEC progenitor cells, which are important for liver injury repair and promoting liver regeneration, but play no role in normal cell turnover; and liver LSEC progenitor cells, which contribute less to liver injury repair and regeneration, but are progenitors for normal LSEC turnover.
The main objective of DeLeve’s study is to find the mechanisms that underlie the dysfunction of repair by bone marrow LSEC progenitor cells to help identify therapeutic targets to facilitate liver regeneration in liver disease.
“The liver is the only solid organ that regenerates,” explained DeLeve. “If you have cancer in your liver, surgeons can remove part of your liver and it can regrow, but it needs the stem cells that we found to do that. What makes this grant so exciting is that we have found pathways that will enhance the liver’s ability to allow these cells to engraft. We’ve also discovered that progenitor cells in the liver and bone marrow are very important for maintaining the endothelial cell population in the liver, and we’re examining their role in aging and various forms of liver disease, including fatty liver disease.”
Borok, professor of medicine and biochemistry and molecular biology and chief of the division of pulmonary, critical care and sleep medicine, and Kahn, received an NIH grant for their study, “Mechanisms of Beta-catenin Signaling in Alveolar Epithelial Cell Differentiation.”
Wnt/beta-catenin signaling, in which signals are passed from outside of a cell through the cell’s surface receptors to inside the cell, plays two apparently opposing roles in lung development and repair following injury: directing progenitor maintenance/expansion, and differentiation. What mechanisms specify each of these divergent roles in any cellular or tissue are mostly unknown.
The alveolar epithelium (alveoli, found in the lung parenchyma, are structures that consist of hollow cavities that act as gas exchange sites) is comprised of two distinct cell populations: type I and type II.
Type II cells serve as optional progenitors for alveolar epithelium maintenance and repair, while type I cells are thought of as terminally differentiated. Injury to the epithelium and failure of regeneration have been implicated in the pathogenesis of a number of chronic lung diseases including lung fibrosis.
The study aims to show how the interactions of beta-catenin with its transcriptional coactivators control the regulation of alveolar type II cell maintenance vs. differentiation during alveolar injury/regeneration. The information Borok and Kahn discover could have an impact on how lungs remodel themselves after an injury, and how chronic diseases such as pulmonary fibrosis progress.
