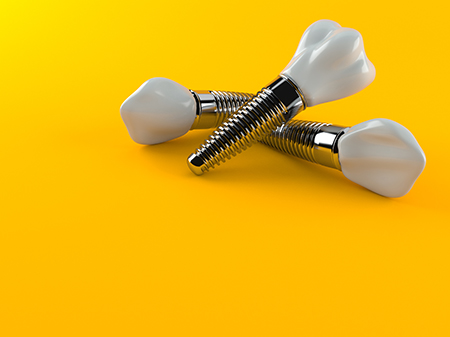
More than 3 million dental implants have been placed in the mouths of U.S. patients, and that number rises by 500,000 each year.
While implants help many people restore their oral health, they come at a cost. Nearly 15 percent of patients with implants develop peri-implantitis, an infectious disease that triggers an immune response of inflammation in the soft and hard tissues surrounding an implant, eventually leading to supporting bone loss. Even more worrying, there is evidence of peri-implant disease within the first three years in 80 percent of patients.
“There is a dramatic risk to the dental profession,” said Malcolm Snead, professor at the Herman Ostrow School of Dentistry of USC. “We can replace lost teeth with implants, but that is putting us in a position where the body is limited in its defense against the implant, and we don’t yet have mechanisms to address the special needs of implants.”
Snead’s research is geared toward battling peri-implantitis by using antimicrobial peptides to inhibit the establishment of bacterial biolfilm. “Our tech wants to level the playing field: innate and adaptive host defenses can continue to operate, but we also can provide an antimicrobial film to potentially kill or inhibit the pathogens associated with periodontal disease,” he explained. These diseases also happen in natural teeth, but because the titanium implant lacks a blood supply, it is a much more susceptible surface for bacterial colonization, Snead said.
In a new paper published in the journal ACS Biomaterials Science & Engineering, Snead and his colleagues report a new machine-learning method to predict the structure of antimicrobial peptides that can target oral keystone pathogens. They also used a peptide with special titanium-binding properties, designed to bind the antimicrobial peptides to the implant’s surface.
Within weeks of an implant being put in a patient’s mouth, biofilm starts to grow, typically starting with four keystone species of pathogens. While systemic antibiotics can treat many types of infections, they can also lead to antibiotic resistance. Instead of a wide-acting antibiotic, the antimicrobial peptide bound to the implant can attack the local bacteria directly.
Eventually, the approach could personalize treatment by identifying each patient’s oral pathogens and direct treatment to those exact bacteria. The new antimicrobial peptide can be applied by the dentist at recall appointments in two minutes, and survives on the implant even after brushing.
Snead worked with an interdisciplinary team from the University of Kansas, led by Professor Candan Tamerler. The team drew from expertise in engineering, structural biology, microbial science and clinical dentistry to develop the peptides.
The application of these principles will allow the team to advance the health of individuals throughout the world.
Snead added that it is particularly pleasing when researchers can translate their biomedical findings to improve oral health and reduce disease.
