Using three-dimensional organ creation, Keck Medicine of University of Southern California (USC) researchers aim to discover clues to metastatic cancer growth by developing a first-ever integrated bioengineered/computational model of metastatic color cancer.
David B. Agus, MD, director of the USC Center for Applied Molecular Medicine and professor of medicine, Keck School of Medicine of USC, is the principal investigator of a $2.3 million, four-year “Provocative Questions” grant awarded recently by the National Cancer Institute (NCI), a division of the National Institutes of Health (NIH). The project title is “An Integrative Computational and Bioengineered Tissue Model of Metastasis.”
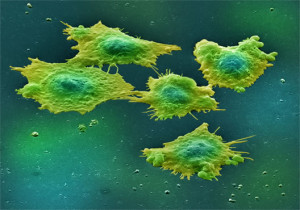
The goal of the research is to develop functional, bioengineered liver “organoids” in which colon cancer tumors can be grown and studied, Agus said. The research team will inject liver “organoids” with cancer cells and watch as the cells grow into tumors and function within the organoids. The research combines bioengineering techniques developed at Wake Forest University with computational models of tumor growth developed at USC.
“Studying cancer metastasis in the lab is problematic because of discrepancies between cell culture models and tumor growth in living organisms,” he said. “We need a much better understanding of the way cancer cells and the organ microenvironment interact. Our research merges the methods of physical science, regenerative medicine and tissue engineering to create a tissue model that approximates the actual environment tumors live.”
The liver models will have value to other cancer researchers seeking to attack tumor growth from different angles, said Shannon Mumenthaler, Ph.D., assistant professor of research in the Department of Medicine at the Keck School and one of the project leads.
“This exciting and novel reproducible, controllable system we are creating will also enable researchers to test hypotheses and make predictions that can be extrapolated to human cancer,” Mumenthaler said.
The first phase of the project involves calibrating the model with data from bioengineered liver tissue. Phase two will subject the growing tumors to physical changes likely to affect them in the human body, including alterations to oxygenation and drug treatment. In the third phase, the team will compare simulations of tumor growth in actual patients with outcome data from these patients.
USC co-authors include Heinz-Josef Lenz, MD, professor of medicine and preventive medicine and associate director for clinical research and co-leader of the Gastrointestinal Cancers program at the Keck School, as well as Paul Macklin, PhD, assistant professor of research, and Dan Ruderman, PhD, assistant professor of research medicine, at the Center for Applied Molecular Medicine. Co-authors from the Wake Forest Institute for Regenerative Medicine (WFIRM) include Anthony Atala, MD, professor and director of WFIRM and chair of the department of urology at Wake Forest University, and Shay Soker, PhD, professor at WFIRM.
The NCI Provocative Questions project was launched in 2012 and is based on 20 important questions from the research community, intended to stimulate researchers to seek out especially effective and imaginative ways to study cancer. According to the NCI, the questions are categorized into five themes: Cancer prevention and risk; mechanisms of tumor development or recurrence; tumor detection, diagnosis and prognosis; cancer therapy and outcomes; clinical effectiveness.
