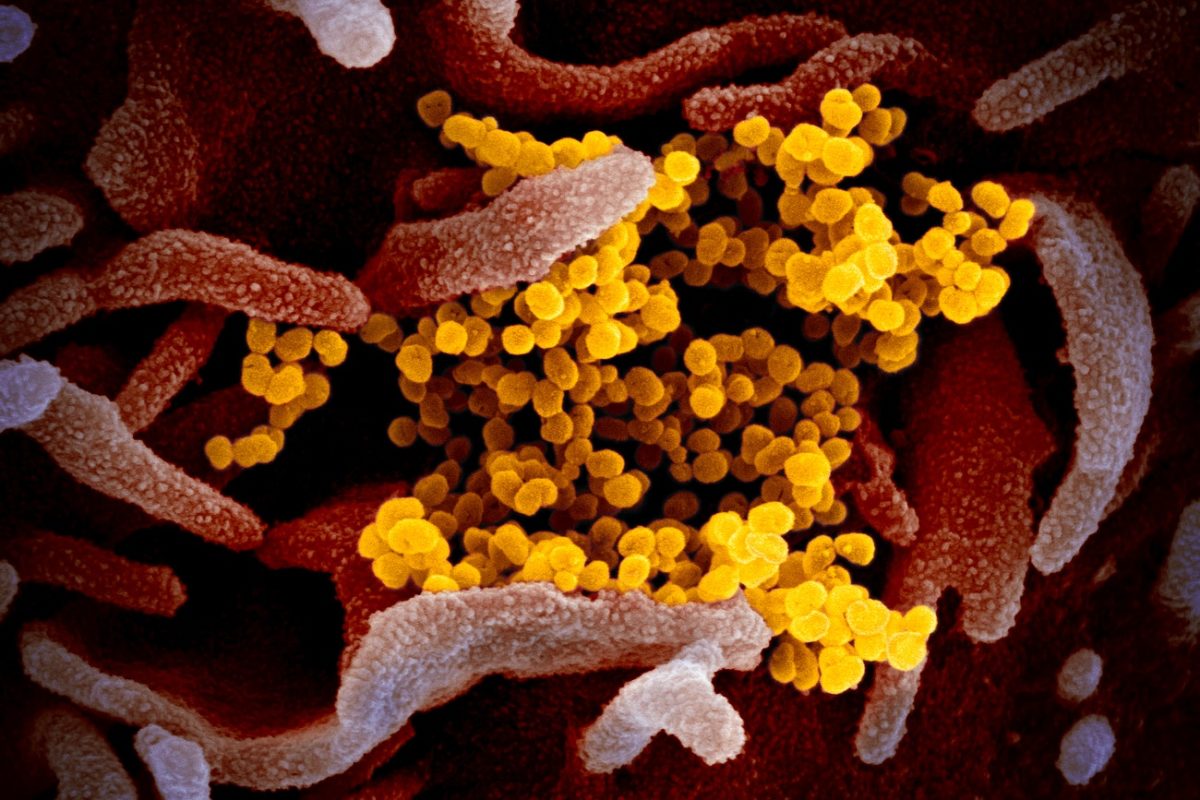
USC scientists are testing out experimental COVID-19 treatments on human “mini-lungs” and lung models, grown in the laboratory using stem cells. With names such as organoids and lung-chips, these simplified, lung-like structures are critically useful for studying infection and for screening large numbers of drug-like molecules to identify promising leads.
Ya-Wen Chen—a new assistant professor of medicine, and stem cell biology and regenerative medicine, and a member of the USC Hastings Center for Pulmonary Research—is using lung organoids to test a potential antiviral treatment to protect against the SARS-CoV-2 coronavirus that causes COVID-19. The antiviral consists of antibodies that block an enzyme called TMPRSS2, which the coronavirus uses to enter the cells lining the lungs via a receptor called ACE2.
To use lung organoids to test another potential antiviral treatment, Chen is collaborating with Justin Ichida, who is the John Douglas French Alzheimer’s Foundation Associate Professor of Stem Cell Biology and Regenerative Medicine at USC and a New York Stem Cell Foundation–Robertson Investigator. Ichida’s team originally identified the potential antiviral, called a kinase, as a drug target for ALS. Blocking the activity of the same kinase also shows promise for protecting lung cells from infection. To support this research, the California Institute for Regenerative Medicine, CIRM, has awarded the team $150,000.
Amy Ryan—an assistant professor of medicine, and stem cell biology and regenerative medicine, and a member of the USC Hastings Center—is studying COVID-19 by using lab-grown lung models, including human Airway Lung-Chips. These structures recapitulate several key characteristics of lung tissue, including airways, blood vessels and blood flow. Ryan’s team is using the Airway Lung-Chip to understand how to modulate the overzealous immune response known as the “cytokine storm” that inflicts severe and even deadly lung damage in certain patients with COVID-19.
To understand another cause of lung damage in COVID-19 patients, Ryan is collaborating with USC scientists Zea Borok, Beiyun Zhou, and Hyungjin Eoh to look at coronavirus infection in the cells of the airway, as well as the cells involved in gas exchange. All of these cells contain networks of membranes, called the endoplasmic reticulum, or ER, which viruses hijack in order to replicate themselves. This hijacking not only allows the virus to multiply, but also stresses out and often kills the lung cells. By studying this stress response, the scientists aim to inform the development of drugs and therapies to inhibit viral replication and lung damage.
Ryan is also leading a multi-disciplinary collaboration to identify genetic risk factors and other biomarkers to predict severe COVID-19 infection, and is providing stem cell-based lung models and pulmonary expertise to several other projects at USC and beyond.
One such project involves Denis Evseenko, an associate professor of orthopaedic surgery, and stem cell biology and regenerative medicine at USC. The Evseenko Lab is studying whether a potential arthritis treatment could also serve as an anti-inflammatory for patients with self-destructive immune reactions to the novel coronavirus.
“When seeking new treatments for a human disease, we need to test these treatments on human cells,” said Andy McMahon, director of the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC. “Stem cells offer one of the very best ways to generate and build relevant models of intricate and vital organs such as the human lung in the laboratory. These models enable us to screen large catalogues of molecules to find promising drug candidates, and to perform detailed studies on actual human cells, as we do our utmost to safely and swiftly end the COVID-19 pandemic.”
