Each year in the U.S., 5,000 patients receive a diagnosis of ALS, an incurable neurodegenerative disease that will likely kill them within two to five years. In the quest to find a cure for these patients, a team of researchers led by USC Stem Cell scientist Justin Ichida has identified two promising avenues for developing new treatments for diverse forms of this devastating disease, which is also known as amyotrophic lateral sclerosis or Lou Gehrig’s disease. Their findings are published in a pair of studies: the first appearing in the journal Cell Stem Cell on February 2, and the second in the journal Cell on February 7.
“A minority of patients have a variety of genetic causes of ALS that can be inherited within families, and a majority have what is known as “sporadic” disease because its causes are unknown,” said Gabriel Linares, a postdoc in the Ichida lab and a co-first author on both studies. “This makes it a difficult challenge to find one treatment that will work for all patients with ALS.”
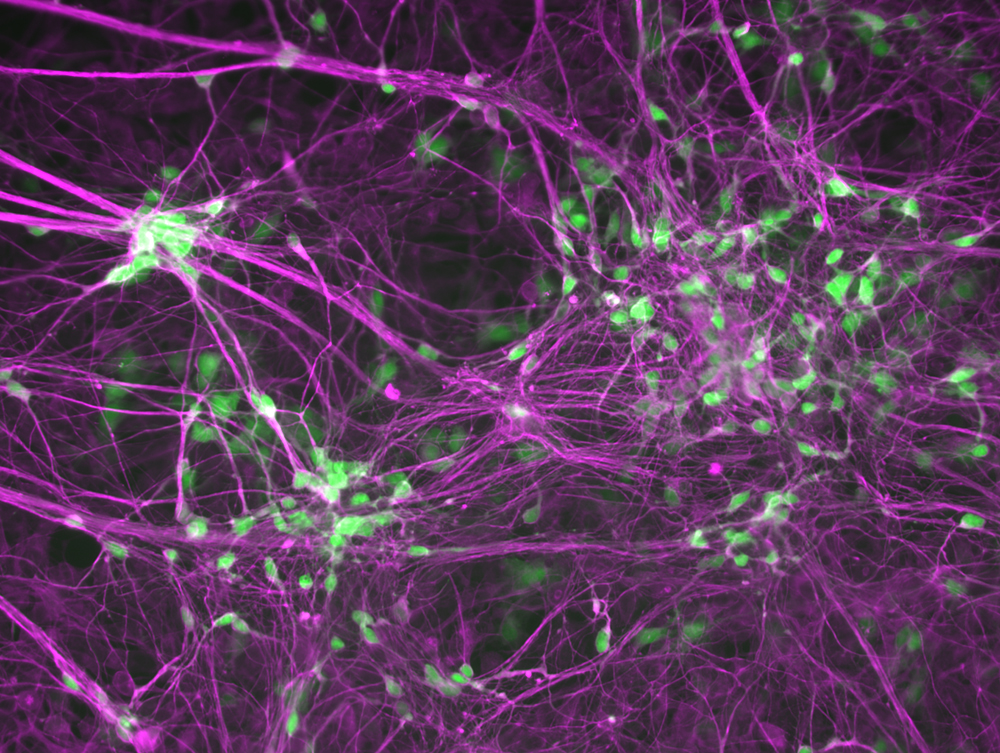
To meet this challenge, the researchers collected skin or blood samples from patients with both familial and sporadic ALS. The scientists reprogrammed the skin and blood cells into motor neurons, which are the nerve cells responsible for movement that degenerate in the disease. These patient-derived motor neurons provided an opportunity to screen thousands of FDA-approved drugs and drug-like molecules to find ones that might be effective against multiple forms of ALS.
In the Cell Stem Cell study, co-first authors Linares and Yichen Li found that several of the most effective drugs and drug-like molecules increased the activity of androgens, the well-known group of sex hormones that include testosterone. However, because androgen-boosting drugs could have undesirable or unsafe side effects for patients with ALS, the scientists aimed to identify a genetic change that might yield similar results.
To accomplish this, they leveraged a public bioinformatics database known as Connectivity Map, developed by the Broad Institute of Harvard and MIT. By analyzing this vast database of information about how drugs affect the genetic landscape underpinning diseases, the scientists accurately predicted that suppressing the SYF2 gene would increase the survival of motor neurons derived from patients with diverse forms of ALS. In addition, suppressing this gene reduced neurodegeneration, motor dysfunction, and other symptoms in mice with ALS.
“What’s really exciting is that SYF2 suppression improved symptoms and pathology related to a protein called TDP-43, which can become toxic and is implicated in close to 97 percent of cases of ALS,” said Li, a postdoc in the Ichida Lab.
In the second study published in Cell, co-first authors Shu-Ting (Michelle) Hung and Linares detail how inhibiting a protein, the PIKFYVE kinase, could represent another effective strategy for treating many different forms of ALS.
In an extensive series of experiments, the researchers inhibited PIKFYVE using the drug apilimod, as well as through genetic and RNA-based approaches, in fruit flies, roundworms, mice, and motor neurons derived from patients with different forms of ALS.
They found that inhibiting PIKFYVE reduced neurodegeneration, improved motor function, and lengthened life by stimulating motor neurons to clear toxic proteins through a process of exocytosis, in which membrane-bound sacs envelop and actively transport waste to the exterior of the cell.
“We were able to pinpoint precisely how PIKFYVE inhibition mitigates neurodegeneration, which is important for informing the development of new targeted treatments,” said Hung, a PhD student in the Ichida Lab.
Ichida, who is the John Douglas French Alzheimer’s Foundation Associate Professor of Stem Cell Biology and Regenerative Medicine at USC, and a New York Stem Cell Foundation–Robertson Investigator, added: “Our discoveries bring us closer to achieving our big picture goal: finding treatments that can be broadly effective for all patients who suffer from ALS.”
Additional co-authors on both studies are: Yunsun Eoh, Manuel Santana, Jonathan Chang, and Joscany Perez from USC; and Wen-Hsuan Chang, Stacee Mendonca, Sarah Hong, and Samuel V. Alworth from AcuraStem, Inc.
For the Cell Stem Cell study, co-authors also include: Hung, Jasper Rubin-Sigler, Wenxuan Guo, Yi-Hsuan Huang, Nomongo Dorjsuren, Michael Chickering, Hao-Jen Deng, Kieu-Tram Bach, and Kamden Gray from USC; Johnny Yu and Hani Goodarzi from the University of California, San Francisco; Tze-Yuan Cheng, Chi Chou Huang, and James Lee from Leica Microsystems; and Jeffrey Rosenfeld from Loma Linda University.
For the Cell study, additional co-authors include: Li, Yingxiao Shi, Sarah Perry, Alexander Couto, Jesse Lai, Eric Hendricks, Yaoming Wang, Berislav V. Zlokovic, and Dion K. Dickman from USC; Gopinath Krishnan and Fen-Biao Gao from the University of Massachusetts; Chuol Kueth, Samantha Macklin-Isquierdo, and Daniela C. Zarnescu from Penn State University; and Sarah Duhaime, Claudia Maios, and J. Alex Parker from the Université de Montréal.
Both studies were supported by federal funding the National Institutes for Health (grants R00NS077435, R01NS097850, 2R01NS097850, R01NS131409, R44NS097094) and U.S. Department of Defense (grants W81XWH-15-1-0187, W81XWH-20-1-0424, W81XWH-21-1- 0168, and W81XWH-21-1-0131). Whole-genome sequencing was provided by the University of Washington Center for Mendelian Genomics with additional federal funding from the NIH (grants UM1 HG006493, U24 HG008956, and S10OD021553). The studies were also supported by private funding from the Donald E. and Delia B. Baxter Foundation, Tau Consortium, Frick Foundation for ALS Research, Muscular Dystrophy Association, New York Stem Cell Foundation, Alzheimer′s Drug Discovery Foundation, Association for Frontotemporal Degeneration, Pape Adams Foundation, John Douglas French Alzheimer′s Foundation, Harrington Discovery Institute, Merkin Family Foundation, USC Broad Innovation Award, Southern California Clinical and Translational Science Institute, and a Broad Postdoctoral Fellowship.
The Cell Stem Cell study received additional support from the California Institute for Regenerative Medicine (CIRM grant DISC2-12158), the ALS Association (grants 22-PDF-588 and 984923, and the Milton Safenowitz Postdoctoral Fellowship), Keck School of Medicine of USC Regenerative Medicine Initiative, and USC Alzheimer′s Disease Research Center.
The Cell study received additional funding from the NIH (grants NS111414, R01NS091299, R37NS057553, R01NS101986, and an NIH Diversity Supplement), CIRM (grant DISC2COVID19-11901), and Target ALS Foundation.
Ichida is co-founder and Alworth is co-founder and CEO of AcuraStem, Inc., and are bound by confidentiality agreements that prevent them from disclosing details of their financial interests in this work. Chang, Mendonca, and Hong are employees of AcuraStem, Inc. Ichida is also a co-founder of Modulo Bio, serves on the scientific advisory boards of AcuraStem, Spinogenix, Synapticure, and Vesalius Therapeutics, and is a paid employee of BioMarin Pharmaceutical. In addition, Zlokovic is a co-founder of ZZ Biotech and chairman of its scientific advisory board, Parker is a co-founder of Modelis, and Gao receives research funding from Stealth BioTherapeutics.
