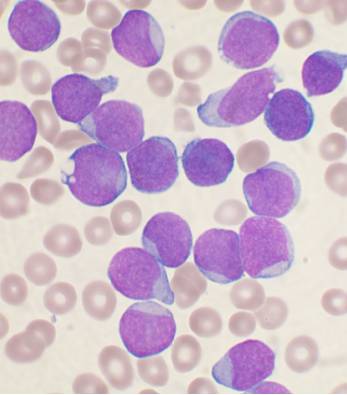
Even within a single patient with cancer, there is a vast diversity of individual tumor cells, which display distinct behaviors related to growth, metastasis, and responses to chemotherapy. To carry out these behaviors, each cancer cell uses its genes to make the needed molecules in a unique way known as its “gene expression signature.” To correlate gene expression signatures with cancer progression and chemotherapy resistance, a team of scientists led by Rong Lu from USC and Akil A. Merchant from Cedars-Sinai have introduced a new genetic technology in a study published in Nature Communications.
To develop the experimental system, first author Humberto Contreras-Trujillo from USC and his colleagues combined two existing technologies. The first enabled the researchers to read the gene expression signatures of individual cancer cells from patients with leukemia. The second technology, developed by the Lu Lab, allowed the scientists to label individual leukemia cells with heritable, DNA-based “barcodes,” offering a way to track not only the cells but also their progeny during disease progression.

Using this experimental system, the team analyzed the gene expression signatures of a representative sample of barcoded leukemia cells, and then transplanted the remainder of the cells into mice.
Distinct gene expression signatures correlated with the various organs where the cancer cells ended up in the mice. For example, cancer cells with high expression of a gene called CMC2 tended to colonize the ovaries, while cells with low levels of CMC2 expression established colonies in the blood and spleen.
Other cancer cells with elevated expression of the genes BTK, DNAJC, and LRIF1 tended to generate progeny in discrete pockets of bone marrow. When the scientists deactivated these genes, leukemia cells accelerated migration, losing their ability to adhere to other cells in the bone marrow.
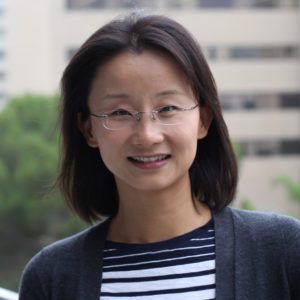
“In our study, we were able to identify previously unknown genes that are involved in disease progression and chemotherapy resistance. These genes may provide new targets for future therapies,” said Lu, who is a Richard N. Merkin Assistant Professor of Stem Cell Biology and Regenerative Medicine, Biomedical Engineering, Medicine, and Gerontology at USC, and a Leukemia & Lymphoma Society Scholar.
By demonstrating that cancer cells with distinct gene expression signatures tend to grow in different organs and bone marrow pockets, the study also underscored a major problem facing cancer researchers: studying non-representative samples of patient cells. For instance, if a physician collects patient cells via a standard blood draw, the sample would not include the non-circulating leukemia cells localized to pockets of the bone marrow. Even more concerning, since these pockets of cancer cells are not uniformly distributed, standard bone marrow biopsies may not accurately diagnose disease in the patient.
There are similar challenges when patient cells are transplanted into laboratory mice in order to conduct pre-clinical cancer research. Less than one percent of the patient cells grow and multiply in mice.
These problems are compounded if patient cells are collected from one mouse, and subsequently transplanted into another mouse. This practice, known as serial transplantation, is a standard technique for allowing small samples of patient cells to expand into the larger quantities needed for research. However, the new Nature Communications study shows that serial transplantations also favor the survival of cancer cells with particular gene expression signatures.
In addition, cells from relapsed patients seemed less likely to survive when transplanted into mice, compared to the cells derived from the same patients prior to any therapeutic treatments. In most cases, the progeny of one or two leukemia cells from the relapsed phase dominated in transplanted mice.
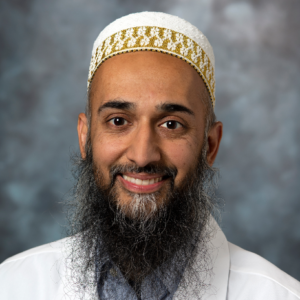
“Our new system laid bare glaring limitations in the leukemia models that are currently used to carry out the final stages of testing before potential therapeutic treatments advance to human clinical trials,” said Merchant, who is a physician-scientist at Cedars-Sinai. “These leukemia models do not capture the full diversity of individual tumor cells within a single patient, let alone within the broader population of patients affected by this disease.”
The researchers also exposed their mice to different variations of the standard leukemia treatment regimen: short-term intensive chemotherapy, followed by long-term maintenance therapy. There were distinct gene expression signatures in leukemia cells that eventually died from intensive treatment, ceased growing due to maintenance therapy, or only responded to a combination of both. Accordingly, in actual clinical practice, combination therapy has proven to be the best overall approach for patients.
“By using our experimental system, we learned a lot about how the gene expression of individual leukemia cells influence their progression and treatment resistance,” said Lu. “The same system can provide similar insights about many other types of cancer, and help identify and characterize the particular cells that drive the disease and underlie treatment resistance.”
Additional co-authors include Jiya Eerdeng, Samir Akre, Du Jiang, Jorge Contreras, Basia Gala, Mary C. Vergel-Rodriguez, Yeachan Lee, Aparna Jorapur, Areen Andreasian, Lisa Harton, Charles S. Bramlett, Anna Nogalska from USC; and Gang Xiao, Jae-Woong Lee, Lai N. Chan, and Markus Müschen from Yale University.
Ninety-five percent of the work was supported by federal funding from the National Heart, Lung, and Blood Institute (grants R35HL150826, R01HL138225, and R01HL135292) and the National Cancer Institute (grants R35CA197628, R01CA213138, R01CA157644, P01CA233412, F31CA206463, and P30CA014089). The remaining 5 percent came from the California Institute for Regenerative Medicine (EDUC2-08381), the Howard Hughes Medical Institute (HHMI-55108547), the University of Southern California Provost’s Undergraduate Research Fellowship, and the Rose Hills Research Fellowship.
