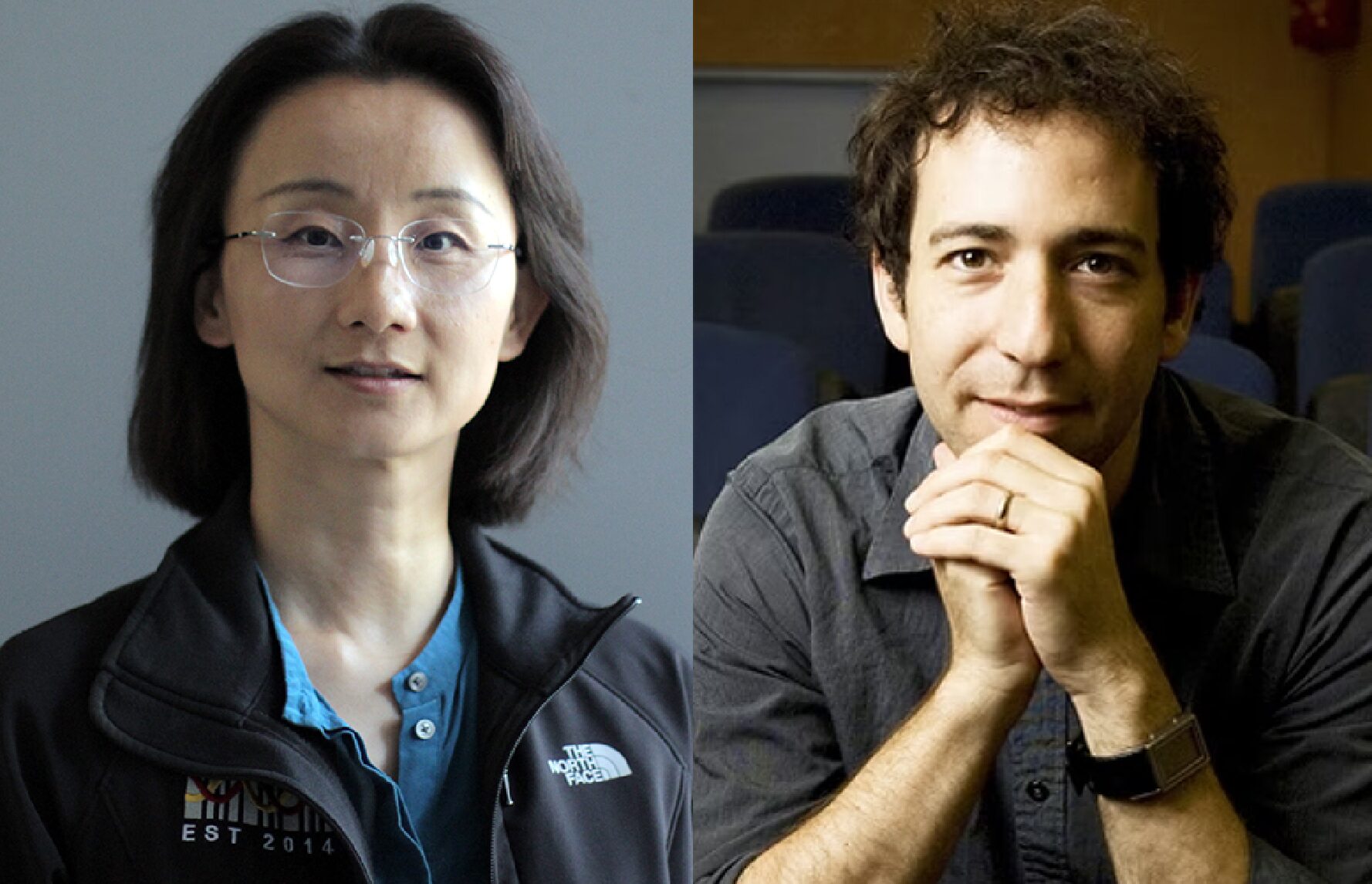
What keeps some immune systems youthful and effective in warding off age-related diseases? In a new paper published in Cellular & Molecular Immunology, USC Stem Cell scientist Rong Lu and her collaborators point the finger at a small subset of blood stem cells, which make an outsized contribution to maintaining either a youthful balance or an age-related imbalance of the two main types of immune cells: innate and adaptive.
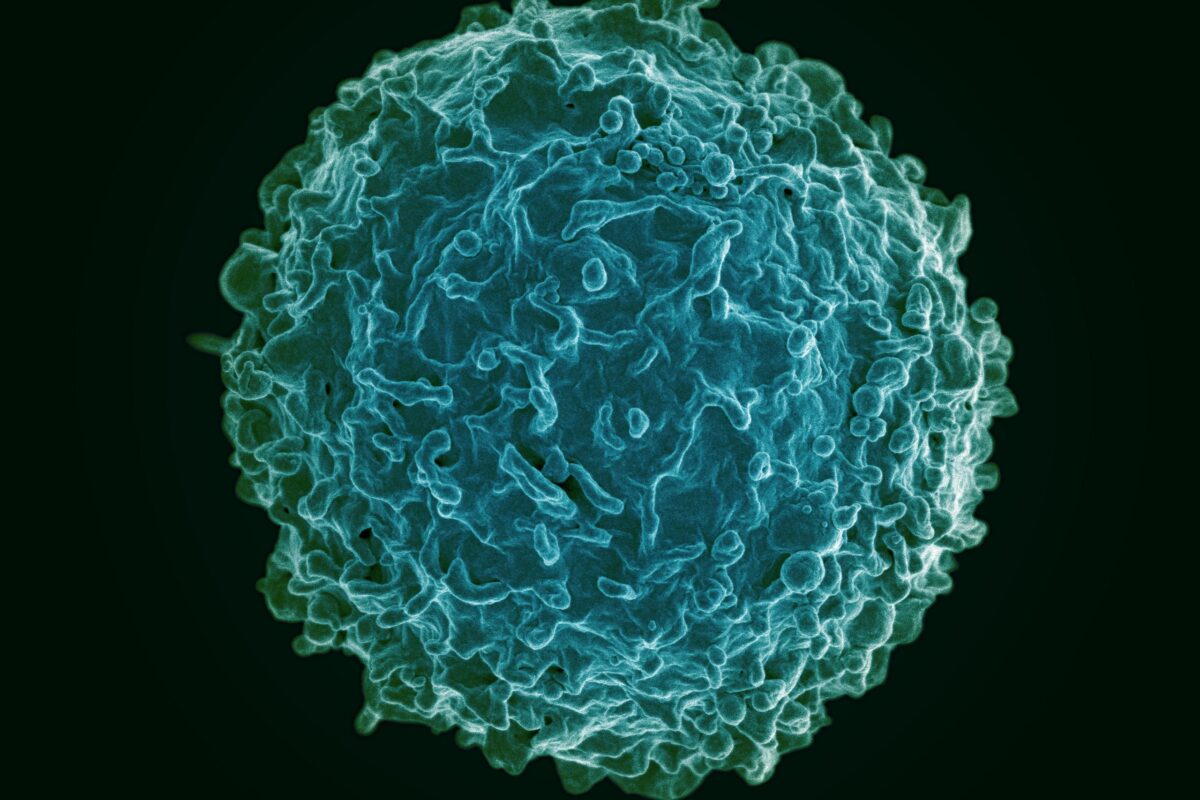
Innate immune cells serve as the body’s first line of defense, mobilizing a quick and general attack against invading germs. For germs that evade the body’s innate immune defenses, the second line of attack consists of adaptive immune cells, such as B cells and T cells that rely on their memory of past infections to craft a specific and targeted response. A healthy balance between innate and adaptive immune cells is the hallmark of a youthful immune system—and a key to longevity.
“Our study provides compelling evidence that when a small subset of blood stem cells overproduces innate immune cells, this drives the aging of the immune system, contributes to disease, and ultimately shortens the lifespan,” said Lu, who is an associate professor of stem cell biology and regenerative medicine, biomedical engineering, medicine, and gerontology at USC, and a Leukemia & Lymphoma Society Scholar. Lu is also a member of the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC, and the USC Norris Comprehensive Cancer Center at the Keck School of Medicine of USC. “Our findings suggest that restraining the small subset of blood stem cells that are overproducing innate immune cells could be an effective way to delay immune aging.”
In the study, first author Anna Nogalska and her colleagues found striking differences in how quickly the immune system ages—even among lab mice with the same genetic background raised in identical conditions. By the advanced age of 30 months, delayed aging mice retained a youthful balance of innate and adaptive immune cells. However, early aging mice showed a big increase in innate immune cells relative to adaptive immune cells.
By tracking the individual blood stem cells responsible for producing both innate and adaptive immune cells, the scientists discovered the subset of blood stem cells primarily responsible for the age-associated imbalance of the immune system. Specifically, the scientists observed that thirty to forty percent of blood stem cells dramatically changed their preference for producing innate versus adaptive immune cells as the mice aged.
In delayed agers, the subset of blood stem cells decreased their production of innate immune cells, protecting against the effects of aging. Among delayed agers, there was an increase in gene activity related to blood stem cells’ regulation and response to external signals—which might keep their production of innate immune cells in check. When the scientists used CRISPR to edit out these genes, blood stem cells reversed their natural tendency and produced more innate immune cells instead of adaptive immune cells—like in the early agers.
In contrast, in early agers, the subset of blood stem cells shifted towards producing more innate immune cells, which, in excess, lead to many diseases of aging. Accordingly, in these early agers, the scientists found an increase in gene activity related to the proliferation of blood stem cells and the differentiation of innate immune cells. When the scientists used CRISPR to edit out these early aging genes, blood stem cells produced more adaptive immune cells instead of innate immune cells—becoming more similar to those in the delayed agers.
Importantly, delayed agers tended to live longer than early agers.
“In the elderly human population, the immune system often tips into producing an overabundance of innate immune cells, which can contribute to diseases such as myeloid leukemia and immune deficiencies,” said Nogalska, senior scientist and lab manager in the Lu Lab. “Our study suggests how we might promote a more youthful immune system to combat these common diseases of aging.”
Additional co-authors are Jiya Eerdeng, Samir Akre, Mary Vergel-Rodriguez, Yeachan Lee, Charles Bramlett, Adnan Y. Chowdhury, Bowen Wang, Colin G. Cess, and Stacey D. Finley from USC.
Ninety percent of the project was supported by federal funding from the National Institutes of Health (grants R00-HL113104, R01HL138225, R35HL150826, and 1F31HL149278-01A1) and the National Cancer Institute (grant P30CA014089). Additional funding came from the California Institute for Regenerative Medicine (grant EDUC4-12756R) and the Leukemia & Lymphoma Society (grant LLS-1370-20).