ALS and frontotemporal dementia (FTD) are two neurodegenerative diseases with a toxic relationship, according to a new USC Stem Cell study published in Nature Medicine.
In the study, Yingxiao TK Shi and Shaoyu Sebastian Lin in the laboratory of Justin Ichida describe how a mutation in a gene, called C9ORF72, leads to toxicity in nerve cells—causing 10 percent of all cases of ALS, and an additional 10 percent of FTD.
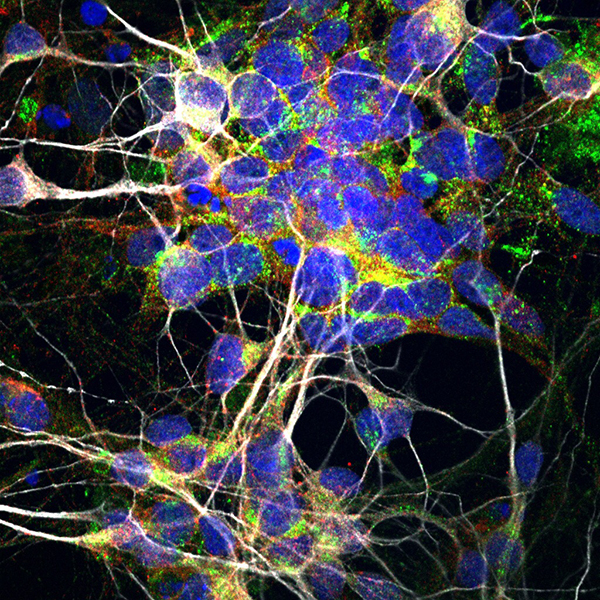
To understand how this happens, the researchers extracted blood from ALS patients carrying the C9ORF72 mutation, and reprogrammed these blood cells into the motor nerve cells that degenerate and die in the disease.
They also extracted blood from healthy patients, reprogrammed these blood cells into motor nerve cells, and used gene editing to delete the C9ORF72 gene.
Whether patient-derived or gene-edited, all motor nerve cells with the mutation had reduced amounts of the protein normally made by the C9ORF72 gene. Furthermore, by adding supplemental C9ORF72 protein, the researchers could stop the motor nerve cells from degenerating.
Through a series of experiments, the researchers revealed that the motor nerve cells use C9ORF72 protein to build lysosomes—which are cellular compartments used to engulf and break down toxic proteins and other garbage.
Without enough lysosomes, the cells accumulate two key types of garbage. The first type is a large, toxic protein produced by the mutated C9ORF72 gene itself. The second type is an excessive number of receptors, or molecules that receive signals from a neurotransmitter known as glutamate. These receptors respond to glutamate by causing the motor nerve cell to activate. Too much activation can kill a motor nerve cell—a phenomenon known as “excitotoxicity.”
Guided by these discoveries, the Ichida Lab is now using patient-derived motor nerve cells to test thousands of potential drugs—with a focus on those that affect lysosomes.
“By understanding the role of lysosomes in ALS and FTD, we can better target our search for new drugs or therapies to treat these devastating diseases,” said Ichida, an assistant professor of stem cell biology and regenerative medicine at USC, and a New York Stem Cell Foundation-Robertson Investigator.
Co-authors include Kim A. Staats, Yichen Li, Wen-Hsuan Chang, Shu-Ting Hung, Eric Hendricks, Gabriel Linares, Yaoming Wang, Brent Wilkinson, Louise Menendez, Toru Sugawara, Phillip Woolwine, Mickey Huang, Michael J. Cowan, Brandon Ge, Nicole Koutsodendris, K. Perry Sandor, Jacob Komberg, Valerie Hennes, Marcelo Coba, and Berislav Z. Zlokovic from USC; Esther Y. Son from Stanford University; Xinmei Wen and Davide Trotti from Thomas Jefferson University; Kassandra Kisler and Amy R. Nelson from USC and Thomas Jefferson University; Vamshidhar R. Vangoor, Ketharini Senthilkumar, Leonard H. van den Berg, and R. Jeroen Pasterkamp from the University Medical Center Utrecht in the Netherlands; Tze-Yuan Cheng and Shih-Jong J. Lee from DRVision Technologies; Paul August from Icagen Corporation; Jason A. Chen, Nicholas Wisniewski, Victor Hanson-Smith, T. Grant Belgard, and Alice Zhang from Verge Genomics; and Chris Grunseich and Michael Ward from the National Institute of Neurological Disorders and Stroke.
Ichida and August are co-founders of Acurastem, Inc.
Seventy-five percent of the research was supported by $6 million of U.S. federal funding from the National Institutes of Health (NIH) (AG039452, AG023084, NS034467, R00NS077435, and R01NS097850) and the Department of Defense (W81XWH-15-1-0187). Twenty-five percent of the work was supported by $2 million from private and non-U.S. sources, including the ALS Foundation Netherlands (TOTALS), Epilepsiefonds (12-08, and 15-05), VICI grant Netherlands Organisation for Scientific Research (NWO), the Donald E. and Delia B. Baxter Foundation, the Tau Consortium, the Frick Foundation for ALS Research, the Muscular Dystrophy Association, the New York Stem Cell Foundation, the Regenerative Medicine Initiative at Keck School of Medicine of USC, the USC Broad Innovation Award, and the Southern California Clinical and Translational Science Institute. Staats received support from a Muscular Dystrophy Association Development Grant, Menendez from an NIH training grant (T32DC009975-04), and Son from a Walter V. and Idun Berry Postdoctoral Fellowship.
