For breast cancer patients, the era of personalized medicine may be just around the corner, thanks to recent advances by USC Stem Cell researcher Min Yu and scientists at Massachusetts General Hospital and Harvard Medical School.
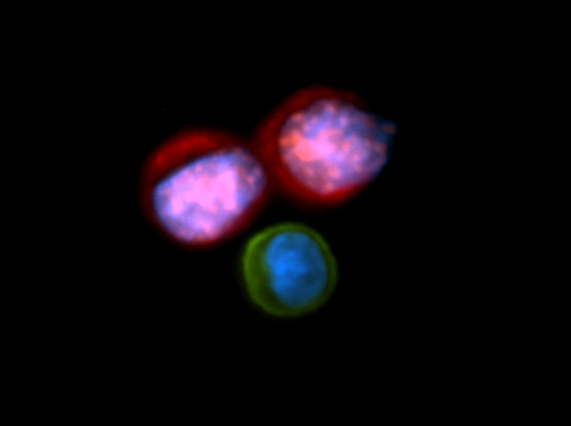
In a July 11 study in Science, Yu and her colleagues report how they isolated breast cancer cells circulating through the blood streams of six patients. Some of these deadly cancer cells are the “seeds” of metastasis, which travel to and establish secondary tumors in vital organs such as the bone, lungs, liver and brain.
Yu and her colleagues managed to expand this small number of cancer cells in the laboratory over a period of more than six months, enabling the identification of new mutations and the evaluation of drug susceptibility.
If perfected, this technique could eventually allow doctors to do the same: use cancer cells isolated from patients’ blood to monitor the progression of their diseases, pre-test drugs and personalize treatment plans accordingly.
In the six estrogen receptor-positive breast cancer patients in the study, the scientists found newly acquired mutations in the estrogen receptor gene (ESR1), PIK3CA gene and fibroblast growth factor receptor gene (FGFR2), among others. They then tested either alone or in combination several anticancer drugs that might target tumor cells with these mutations and identified which ones merit further study. In particular, the drug Ganetspib — also known as STA-9090 — appeared to be effective in killing tumor cells with the ESR1 mutation.
“Metastasis is the leading cause of cancer-related death,” said Yu, assistant professor in the Department of Stem Cell Biology and Regenerative Medicine at the Keck School of Medicine of USC. “By understanding the unique biology of each individual patient’s cancer, we can develop targeted drug therapies to slow or even stop their diseases in their tracks.”
Additional co-authors include Aditya Bardia, Nicola Aceto, Francesca Bersani, Marissa W. Madden, Maria C. Donaldson, Rushil Desai,Huili Zhu, Valentine Comaills, Zongli Zheng, Ben S. Wittner, Petar Stojanov, Elena Brachtel, Dennis Sgroi, Ravi Kapur, Toshihiro Shioda, David T. Ting, Sridhar Ramaswamy, Gad Getz, A. John Iafrate, Cyril Benes, Mehmet Toner, Shyamala Maheswaran and Daniel A. Haber.
This work was supported by grants from the Breast Cancer Research Foundation, Stand Up to Cancer, the Wellcome Trust, National Foundation for Cancer Research, National Institutes of Health CA129933, National Institute of Biomedical Imaging and Bioengineering EB008047, Susan G. Komen for the Cure KG09042, National Cancer Institute–MGH Proton Federal Share Program, the MGH-Johnson and Johnson Center for Excellence in CTCs, and the Howard Hughes Medical Institute.
