A new study by researchers at Children’s Hospital Los Angeles (CHLA) has shown that neonatal mouse hearts have varying regenerative capacities depending upon the severity of injury. Using cryoinjury — damaging the heart through exposure to extreme cold in order to mimic cellular injury caused by myocardial infarction — investigators found that neonatal mouse hearts can fully recover normal function following a mild injury, though fail to regenerate after a severe injury.
Published online by the journal Developmental Biology, the study suggests that cardiac regeneration strategies should be based on the type and severity of heart injury.
“Using models such as zebrafish and neonatal mice that regenerate their hearts naturally, we can begin to identify important molecules that enhance heart repair,” said Ellen Lien of The Saban Research Institute of Children’s Hospital Los Angeles. Lien, who was senior author on the paper, is also an assistant professor at the Keck School of Medicine of USC and a principal investigator with USC Stem Cell.
Newborn mice have shown the capacity for heart regeneration, but it is rapidly lost by seven days after birth. Approaches to extend this regenerative capacity in a mammalian model, from the neonatal period to the juvenile or adult period, could help identify new treatment options for humans.
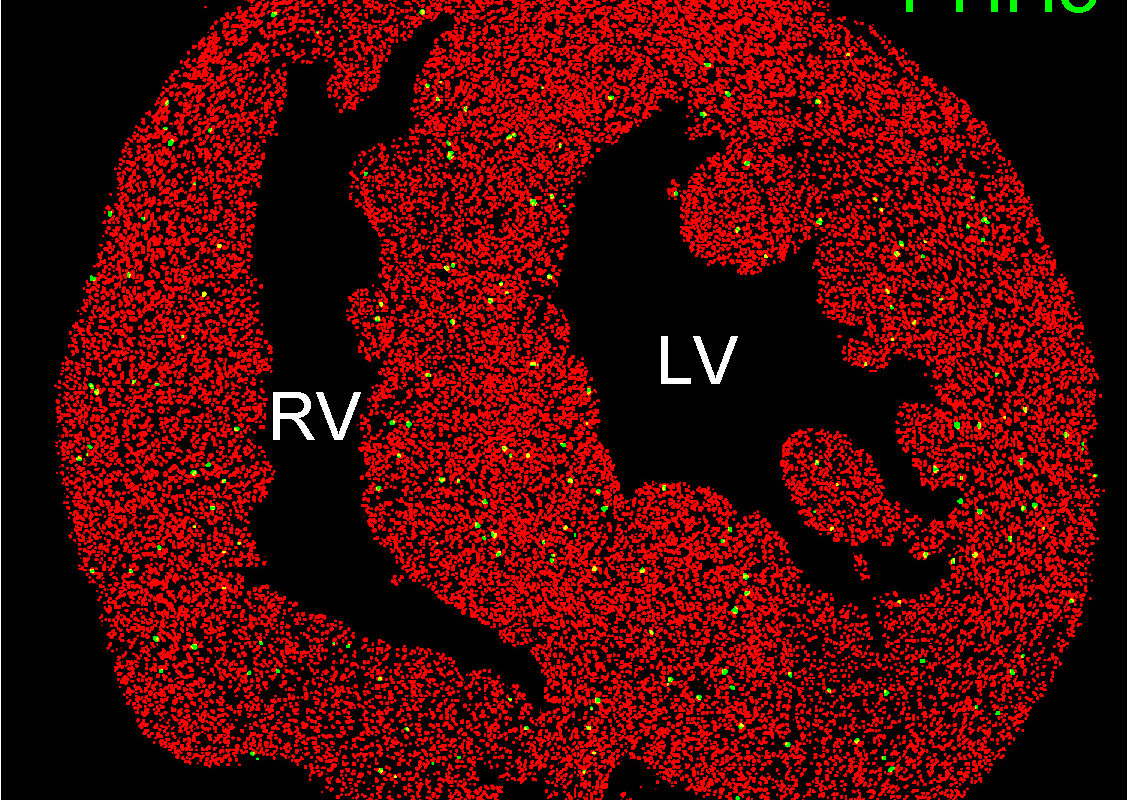
Acute myocardial infarction, commonly known as a heart attack, can be classified according to the extent of damage to the heart muscle. Severe, or transmural injury, is associated with a blood supply blockage to the full thickness of the heart. Non-transmural injury indicates a blockage that penetrates only partially through the heart muscle. The investigators were able to develop models for both types of injury.
In addition to differences in regenerative capacity, the investigators also found an indicator of tissue fibrosis or “scarring,” profibrotic marker PAI-1, was markedly elevated only after transmural injury. In both models post-injury, the cells that form heart muscle, cardiomyocytes, did not increase significantly. However, responses to cardiac injury repair in the outer layer of the heart (epicardium) and blood vessels (revascularization) were present.
“If we can figure out how to activate this youthful type of myocardial regeneration program in humans, it will be a major clinical breakthrough,” said David Warburton, director of Developmental Biology and Regenerative Medicine at The Saban Research Institute of CHLA. Warburton is also a member of the USC Stem Cell Executive Committee, a professor at the Keck School of Medicine of USC and a co-author on the paper.
Additional contributors include Ali Darehzereshki, Nicole Rubin, Laurent Gamba, Jieun Kim, James Fraser, Ying Huang, Joshua Billings, John Wood, The Saban Research Institute of CHLA; Robabeh Mohammadzadeh, Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC; Vesa Kaartinen, University of Michigan.
Funding was provided in part by the National Heart, Lung and Blood Institute R01HL096121, The Saban Research Institute Career Development Award, and the California Institute for Regenerative Medicine (CIRM) postdoctoral fellowship TG2-01168.
