Can the same gene prevent and promote cancer? When it comes to liver cancer, the gene that codes for P53, a protein found in humans and many other animals, involves this catch-22.
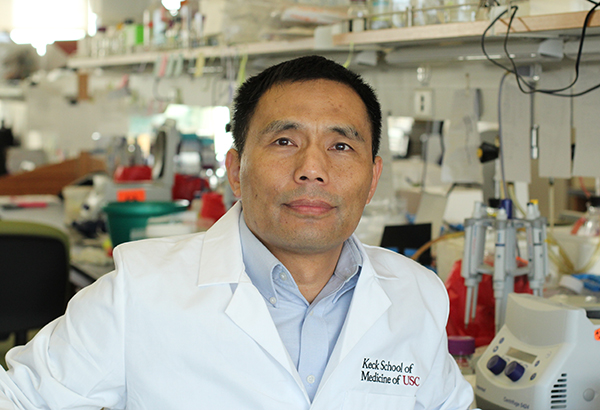
In a pair of articles published in Oncogene and the Journal of Hepatology, USC faculty member Qi-Long Ying and a team of researchers revealed that P53 can both help and harm a liver exposed to carcinogenic chemicals.
The good news: P53 serves as a guardian against tumors by inducing potentially pre-cancerous liver cells to “commit suicide” or go into growth arrest. The bad news: These dying cells can trigger inflammation, which in turn can promote a cancer known as hepatocellular carcinoma (HCC).
In humans, common causes of HCC include exposure to viruses such as Hepatitis B, which is especially prevalent in East Asia and sub-Saharan Africa. Liver cancer is a leading cause of cancer-related death worldwide.
As reported in Oncogene, Ying’s team studied this prevalent form of cancer by genetically engineering rats with abnormally low levels of P53 and comparing them to regular rats. When chronically exposed to a chemical known to cause liver cancer, the P53-deficient rats surprised the researchers by faring better than their normal peers, exhibiting less inflammation and cirrhosis, as well as fewer liver tumors.
Building on these findings, an article in the Journal of Hepatology suggested there may be a way to reap the benefits of P53’s guardian functions while avoiding chronic, cancer-promoting inflammation. That’s because P53 itself doesn’t cause inflammation directly, but rather by triggering the release of a highly inflammatory molecule called HMGB1. When exposed to carcinogens, rats developed less cirrhosis and fewer liver tumors if they were also given ethyl pyruvate, an anti-inflammatory that blocks HMGB1 but doesn’t interfere with P53’s beneficial functions.
“In these two papers, we’ve discovered a dark side of the gene that codes for P53 — which a lot of people think is a good gene,” Ying said. “But you cannot just simply say a gene is good or bad. Every gene can do bad things and can also do good things, depending on the environment. So P53 actually promotes tumorigenesis in the particular case described in our paper.”
As researchers continue to study HCC and other cancers, the P53-deficient rat, produced using genetic material from rat embryonic stem cells, will continue to provide useful insights.
Ying, associate professor of cell and neurobiology at the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC, collaborated with several colleagues on these studies. Co-authors on both studies include He-Xin Yan, Hong-Ping Wu, Charles Ashton and Chang Tong from the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC and Hui-Lu Zhang, Han Wu, Qi-Jun Qian and Hong-Yang Wang from the Second Military Medical University in Shanghai. Yan and Wu are also affiliated with the Second Military Medical University.
The National Institutes of Health provided funding for these projects (grant number R01OD010926). The Program for Professor of Special Appointment (Eastern Scholar) at Shanghai Institutions of Higher Learning provided additional support for the research published in the Journal of Hepatology.
