The lymph nodes, liver and kidney are not passive filters for toxins, but complex organ systems that perform an astonishing array of critical functions. To help patients who have suffered damage to these organ systems, this year’s Broad Clinical Research Fellows are pioneering new regenerative strategies.
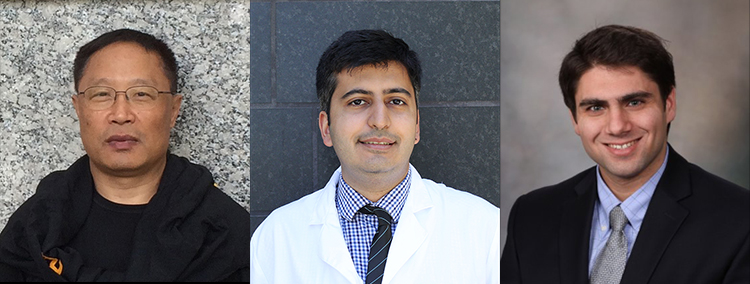
As a clinical nephrology fellow at USC, Roshan Rajani will research regenerative approaches to treating chronic kidney disease (CKD), which affects more than 30 million patients in the US. CKD can develop due to long-term damage to the kidney’s delicate blood vessels inflicted by diabetes or high blood pressure, or following an episode of acute kidney injury. CKD often progresses to end-stage kidney disease, a grave condition requiring painful dialysis or organ transplantation.
As a potential therapy for patients with CKD, Rajani will explore the body’s pH as a tool for boosting its population of regenerating kidney cells. Several studies have shown that patients with CKD have overly acidic blood, and that an alkaline diet can slow the progression of their disease. Follow-up studies suggested that alkalinity increases the activity of an enzyme called AMP-activated protein kinase (AMPK), which might be important for kidney regeneration.
Building on these promising findings, Rajani will feed mice with CKD baking soda to increase their blood alkalinity. In follow-up experiments, he will treat mice with the drug metformin to directly stimulate AMPK activity, before feeding them baking soda.
“We hypothesize that combining these two therapies, alkali and metformin, offers additive kidney protection in CKD,” said Rajani. “If our hypothesis is correct, we may open a new therapeutic avenue for patients with CKD. I’d like to thank The Broad Foundation for their support.”
Rajani will perform this research under the mentorship of Nuria M. Pastor-Soler, associate professor of medicine in the USC/UKRO Kidney Research Center and the Division of Nephrology and Hypertension at the Keck School of Medicine of USC. She is also the assistant dean for research mentoring.
A second Broad Clinical Research Fellow, Anthony I. Squillaro, will study regenerative strategies to treat liver disease.
Approximately 30 million people worldwide, and one in 10 people in the US, suffer from liver disease. If this progresses to end-stage liver failure, patients require organ transplantation, and don’t receive much relief from conventional cell replacement therapies. So far, liver cells or stem cells—injected directly into the organ or housed in devices—have only survived for one to 12 months, and there are not enough donor organs to continually replenish the supply.
Squillaro aims to develop an alternative approach: tissue-engineered liver (TELi), grown from a patient’s own stem cells. First, Squillaro will optimize the formation of TELi from stem cell-derived, organ-like structures known as hepatoblasts, and then deliver these hepatoblasts to mice as a treatment for liver failure. He will determine the best dose of hepatoblasts, as well as the amount of time that it takes for them to develop into functional TELi. Most importantly, he will investigate whether TELi can survive long-term in mice, and rescue them from liver failure.
“The overall objective of this project is to develop and investigate whether TELi is a more robust and effective cell therapy for the treatment of liver disease,” said Squillaro, a clinical resident and postdoctoral fellow in the Department of Pediatric Surgery at Children’s Hospital Los Angeles (CHLA). “I’m grateful to The Broad Foundation for supporting me in furthering stem cell therapies for surgical patients.”
Squillaro will conduct his research in the laboratory of Tracy C. Grikscheit, principal investigator with USC Stem Cell and The Saban Research Institute of CHLA. Grikscheit is also an attending surgeon and associate professor of surgery at CHLA, with appointments at the Keck School and the USC Viterbi School of Engineering.
A clinical fellow in USC’s Department of Surgery, Wan Jiao will work to develop a stem cell-based treatment for lymphedema, or swollen limbs resulting from the removal of cancerous lymph nodes.
To test a new approach to treating this painful condition, Jiao intends to implant stem cells onto a special scaffold into the limbs of rats with lymphedema. The stem cells will hopefully develop into new lymph nodes and channels to drain the swelling.
“There are a number of lymphedemas that are very difficult to repair and lack satisfactory solutions,” said Jiao. “My goal with this fellowship is to determine whether reprogramming stem cells to overproduce lymphatic cells can help heal lymphedema in animals and, ultimately, provide a better alternative for repair in humans.”
He’ll work under the mentorship of Young Kwon Hong and Alex Wong, two faculty members in the Department of Surgery.
Jiao, Squillaro and Rajani are part of a distinguished group of Broad Clinical Fellows at USC, the University of California, Los Angeles (UCLA) and the University of California, San Francisco (UCSF)—which all have stem cell research centers established with support from Eli and Edythe Broad and the California Institute for Regenerative Medicine (CIRM).
At these sister stem cell research centers, The Eli and Edythe Broad Foundation has funded clinical fellowships for the past three years. The fellowships support clinicians performing full-time research related to stem cell biology and regenerative medicine, with $65,000 of salary support, $7,500 for supplies and a $1,500 meeting allowance. Each fellowship is potentially renewable for a second year.
“Physician-scientists are essential partners as we translate our stem cell advances into new strategies for patient care,” said Andy McMahon, director of the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC. “By supporting our talented and hard-working clinical fellows, the Broads are making a visionary investment in the medicine of the future.”
